Diabetes is a chronic metabolic disorder characterized by impaired glucose processing in the body. Glucose serves as a primary energy source for cellular functions. The condition encompasses three main types: Type 1, Type 2, and gestational diabetes.
Type 1 diabetes results from an autoimmune response in which the immune system destroys insulin-producing beta cells located in the pancreas. While this condition typically emerges during childhood or adolescence, onset can occur at any age. Individuals with Type 1 diabetes produce insufficient or no insulin, requiring continuous insulin replacement therapy for blood glucose regulation.
Type 2 diabetes represents the most common form of the disease and predominantly affects adults, though increasing rates of childhood obesity have led to more frequent diagnoses in younger populations. This condition involves either insulin resistance, where cells fail to respond effectively to insulin, or inadequate insulin production by the pancreas. Multiple factors influence Type 2 diabetes development, including genetic susceptibility, dietary patterns, physical activity levels, and environmental exposures.
Gestational diabetes develops during pregnancy and generally resolves following delivery. However, women who experience gestational diabetes face elevated risks for developing Type 2 diabetes in subsequent years. Several factors contribute to diabetes development.
Genetic inheritance significantly influences susceptibility, with family history serving as a notable risk factor. Lifestyle elements including high-calorie diets, sedentary behavior, and excess body weight substantially increase diabetes risk. Medical conditions affecting hormone production and certain medications can also impair insulin function or glucose metabolism.
Recognition of these risk factors enables implementation of preventive measures and appropriate disease management strategies.
Key Takeaways
- Diabetes has multiple types with varied causes, requiring tailored management approaches.
- Healthy diet and regular exercise are crucial lifestyle changes to control diabetes effectively.
- Medication, including insulin and oral drugs, plays a key role in managing blood sugar levels.
- Continuous glucose monitoring offers real-time data, improving diabetes control and decision-making.
- Mental health and stress management significantly impact diabetes outcomes and should be addressed.
Lifestyle Modifications: Diet and Exercise
Making lifestyle modifications is essential for managing diabetes effectively. Your diet plays a pivotal role in controlling blood sugar levels. A balanced diet rich in whole grains, lean proteins, healthy fats, fruits, and vegetables can help you maintain stable glucose levels.
It’s important to monitor your carbohydrate intake since carbohydrates have the most significant impact on blood sugar. You might find it beneficial to work with a registered dietitian who can help you create a personalized meal plan that aligns with your health goals. In addition to dietary changes, incorporating regular physical activity into your routine can significantly improve your overall health and help manage diabetes.
Exercise enhances insulin sensitivity, allowing your body to use glucose more effectively. Aim for at least 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking or cycling. Strength training exercises are also beneficial as they help build muscle mass, which can further improve glucose metabolism.
Finding activities you enjoy will make it easier to stick with your exercise routine. Making these lifestyle changes may seem daunting at first, but small, gradual adjustments can lead to significant improvements over time. You might start by setting achievable goals, such as cooking one healthy meal per week or taking a short walk after dinner.
As you become more comfortable with these changes, you can gradually increase their intensity and frequency. Remember that consistency is key; over time, these modifications will become second nature and contribute positively to your overall well-being.
Medication Management: Insulin and Oral Medications

For many individuals with diabetes, lifestyle modifications alone may not be sufficient to maintain optimal blood sugar levels. In such cases, medication management becomes essential. Insulin therapy is often necessary for those with Type 1 diabetes since their bodies cannot produce insulin.
There are various types of insulin available, each with different onset times and durations of action. Your healthcare provider will work with you to determine the best regimen based on your individual needs and lifestyle. For those with Type 2 diabetes, oral medications may be prescribed to help manage blood sugar levels.
These medications work in various ways; some increase insulin sensitivity, while others stimulate the pancreas to produce more insulin or reduce glucose production by the liver. It’s important to understand how each medication works and its potential side effects. Regular communication with your healthcare provider will ensure that your treatment plan remains effective and that any necessary adjustments are made promptly.
Managing diabetes through medication requires diligence and commitment. You should take your medications as prescribed and monitor your blood sugar levels regularly to assess their effectiveness. If you experience any side effects or have concerns about your medications, don’t hesitate to discuss them with your healthcare provider.
They can provide guidance and support to help you navigate any challenges you may encounter along the way.
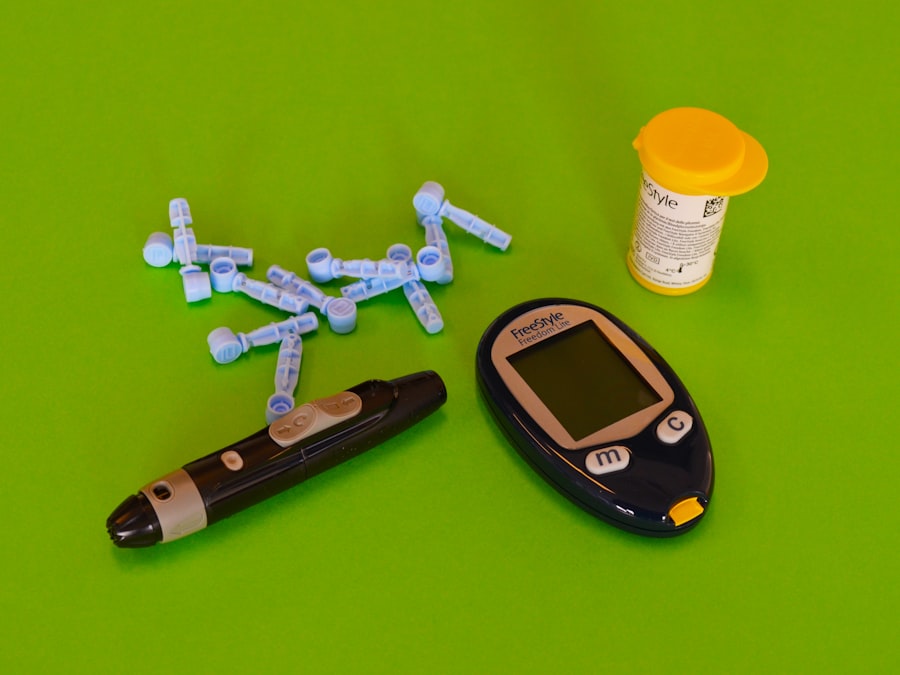
Continuous Glucose Monitoring: Benefits and Usage
Continuous glucose monitoring (CGM) has revolutionized diabetes management by providing real-time data on blood sugar levels throughout the day and night. This technology involves wearing a small sensor that measures glucose levels in the interstitial fluid just beneath the skin. The data collected is transmitted to a device or smartphone app, allowing you to track fluctuations in your blood sugar levels continuously.
One of the primary benefits of CGM is its ability to provide insights into how different foods, activities, and stressors affect your glucose levels. With this information at your fingertips, you can make more informed decisions about your diet and lifestyle choices. For instance, if you notice that certain foods cause significant spikes in your blood sugar, you can adjust your eating habits accordingly.
Additionally, CGM can alert you to potential hypoglycemic episodes before they become severe, allowing you to take corrective action promptly. While CGM offers numerous advantages, it’s essential to understand how to use this technology effectively. Familiarize yourself with the device’s features and settings to maximize its benefits.
Regularly calibrating the sensor as instructed will ensure accurate readings. Moreover, integrating CGM data into your overall diabetes management plan will empower you to take control of your health proactively.
Stress Management and Mental Health: Impact on Diabetes
| Metric | Description | Target Range | Measurement Frequency |
|---|---|---|---|
| HbA1c (Glycated Hemoglobin) | Average blood glucose over past 2-3 months | Below 7% | Every 3-6 months |
| Fasting Blood Glucose | Blood sugar level after at least 8 hours of fasting | 80-130 mg/dL | Daily or as recommended |
| Postprandial Blood Glucose | Blood sugar level 1-2 hours after meals | Less than 180 mg/dL | Daily or as recommended |
| Blood Pressure | Pressure of blood in arteries | Below 130/80 mmHg | Regularly at each visit |
| Body Mass Index (BMI) | Weight-to-height ratio to assess obesity | 18.5 – 24.9 kg/m² | Every visit |
| Lipid Profile | Cholesterol and triglyceride levels | LDL: Below 100 mg/dL HDL: Above 40 mg/dL (men), 50 mg/dL (women) Triglycerides: Below 150 mg/dL |
Annually or as recommended |
| Kidney Function (eGFR, Albuminuria) | Assessment of kidney health | eGFR: Above 60 mL/min/1.73m² Albuminuria: Less than 30 mg/g |
Annually |
| Foot Examination | Check for ulcers, neuropathy, and circulation | No ulcers or infections | At least annually |
Managing diabetes goes beyond physical health; mental well-being plays a crucial role in how effectively you can manage the condition. Stress can significantly impact blood sugar levels by triggering hormonal responses that lead to increased glucose production in the liver. When you’re under stress, you may find it challenging to adhere to your diet or exercise routine, which can further complicate diabetes management.
Recognizing the connection between stress and diabetes is vital for maintaining balance in your life. You might consider incorporating stress-reduction techniques into your daily routine, such as mindfulness meditation, yoga, or deep-breathing exercises. These practices can help lower stress levels and improve your overall mental health.
Additionally, seeking support from mental health professionals or joining support groups can provide valuable coping strategies and emotional support. It’s essential to prioritize self-care as part of your diabetes management plan. Engaging in activities that bring you joy and relaxation can help mitigate stress and improve your overall quality of life.
Whether it’s spending time with loved ones, pursuing hobbies, or simply taking time for yourself, these moments of respite are crucial for maintaining both mental and physical health.
Importance of Regular Monitoring and Check-ups
Regular monitoring of blood sugar levels is a cornerstone of effective diabetes management. By keeping track of your glucose levels consistently, you can identify patterns and make informed decisions about your diet, exercise, and medication adjustments. You might find it helpful to keep a log of your readings alongside notes about what you ate or how active you were that day; this information can provide valuable insights when discussing your management plan with healthcare providers.
In addition to self-monitoring, regular check-ups with your healthcare team are essential for comprehensive diabetes care. These appointments allow for ongoing assessment of your condition and provide opportunities for education about new management strategies or technologies that may benefit you. During these visits, healthcare professionals can also monitor for potential complications associated with diabetes, such as cardiovascular issues or neuropathy.
Establishing a routine for check-ups can help ensure that you stay on track with your health goals. You might consider scheduling appointments at regular intervals—such as every three months—to maintain consistent oversight of your condition. This proactive approach will empower you to take charge of your health while fostering a collaborative relationship with your healthcare team.
Support Systems: Family, Friends, and Diabetes Community
Navigating life with diabetes can be challenging; however, having a strong support system can make a significant difference in how you manage the condition. Family and friends play an essential role in providing emotional support and encouragement as you work towards maintaining healthy habits. Sharing your experiences with loved ones can foster understanding and empathy while helping them learn how best to support you.
In addition to personal relationships, connecting with others who share similar experiences through diabetes support groups or online communities can be incredibly beneficial. These platforms offer opportunities for sharing tips, resources, and encouragement while also providing a sense of belonging. Engaging with others who understand the challenges of living with diabetes can alleviate feelings of isolation and empower you on your journey toward better health.
Building a robust support network takes time and effort; however, the rewards are invaluable. By surrounding yourself with individuals who uplift and motivate you, you’ll find it easier to stay committed to managing your diabetes effectively while also enhancing your overall quality of life.
Future Trends in Diabetes Management: Technology and Research
The landscape of diabetes management is continually evolving thanks to advancements in technology and ongoing research efforts aimed at improving care for individuals living with this condition. One exciting trend is the development of artificial intelligence (AI) systems that analyze data from continuous glucose monitors and other devices to provide personalized recommendations for managing blood sugar levels more effectively. Additionally, research into new medications and treatment options continues to expand the possibilities for diabetes management.
For instance, studies are exploring innovative approaches such as gene therapy or immunotherapy that could potentially alter the course of Type 1 diabetes or improve insulin sensitivity in those with Type 2 diabetes. As technology continues to advance, staying informed about new developments will empower you to make educated decisions regarding your care plan. Embracing these innovations may enhance not only how you manage diabetes but also improve overall health outcomes in the long run.
By remaining proactive about learning and adapting to new trends in diabetes management, you’ll be better equipped to navigate this journey successfully while maintaining a fulfilling life.

