Bone density refers to the amount of mineral matter per square centimeter of bone. It is a crucial indicator of bone health, as it reflects the strength and structural integrity of your bones. High bone density typically means that your bones are strong and less likely to fracture, while low bone density can lead to an increased risk of breaks and other complications.
Understanding bone density is essential for maintaining overall health, especially as you age. As you grow older, your body undergoes various changes, including alterations in bone density. Peak bone mass is usually reached in your late twenties to early thirties, after which bone resorption begins to outpace bone formation.
This natural process can lead to a gradual decline in bone density over time. Therefore, being aware of your bone health and taking proactive measures to maintain it is vital for preventing future issues.
Key Takeaways
- Bone density measures the strength and health of bones, crucial for overall skeletal integrity.
- Genetics, diet, physical activity, and hormonal changes significantly influence bone density.
- Osteoporosis is a condition characterized by weakened bones and increased fracture risk.
- Key risk factors include age, gender, family history, and lifestyle choices like smoking and low calcium intake.
- Prevention and management involve a balanced diet, regular exercise, medication, and lifestyle adjustments.
Factors Affecting Bone Density
Several factors influence your bone density, and understanding these can empower you to take control of your bone health. Genetics plays a significant role; if your family has a history of osteoporosis or fractures, you may be at a higher risk. Additionally, your sex can impact your bone density, as women generally have lower bone density than men, particularly after menopause due to hormonal changes that affect bone metabolism.
Lifestyle choices also significantly affect your bone density. Diet is a critical factor; consuming adequate amounts of calcium and vitamin D is essential for maintaining strong bones. Calcium is the primary mineral found in bones, while vitamin D helps your body absorb calcium effectively.
Regular physical activity, particularly weight-bearing exercises, can also enhance bone density by stimulating bone formation and slowing down the rate of bone loss. Conversely, smoking and excessive alcohol consumption can negatively impact your bone health, leading to decreased density over time.
Understanding Osteoporosis

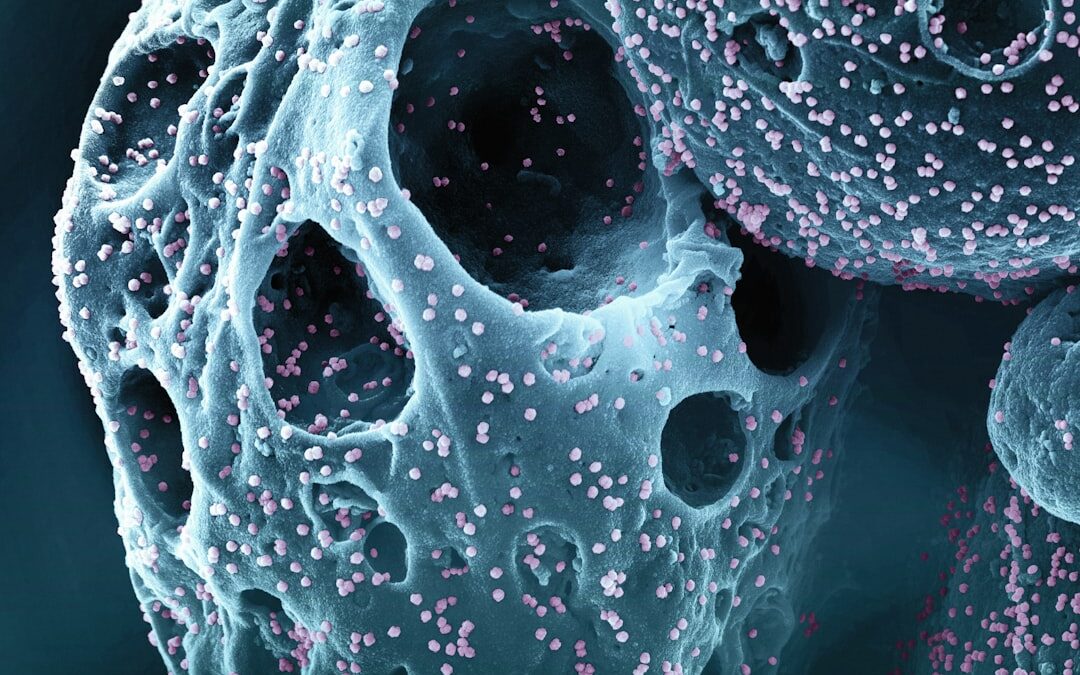
Osteoporosis is a condition characterized by weakened bones that are more susceptible to fractures. It often develops silently over many years, making it difficult to detect until a fracture occurs. The term “osteoporosis” literally means “porous bones,” which describes the structural changes that occur within the bone tissue as it loses density.
This condition can affect anyone but is particularly prevalent among older adults, especially postmenopausal women. The progression of osteoporosis can be insidious; you may not experience any symptoms until a fracture occurs. Common sites for fractures include the hip, spine, and wrist.
These fractures can lead to significant pain, disability, and a decreased quality of life. Understanding osteoporosis is crucial for recognizing its potential impact on your health and taking steps to mitigate its effects.
Risk Factors for Osteoporosis
Identifying risk factors for osteoporosis is essential for prevention and early intervention. Age is one of the most significant risk factors; as you age, your bones naturally become less dense. Gender also plays a role, with women being at a higher risk due to hormonal changes during menopause that accelerate bone loss.
Additionally, family history can increase your susceptibility; if osteoporosis runs in your family, you may need to be more vigilant about monitoring your bone health. Other lifestyle-related factors can also contribute to your risk of developing osteoporosis. A diet low in calcium and vitamin D can hinder your body’s ability to maintain strong bones.
Sedentary behavior, such as prolonged periods of inactivity or lack of weight-bearing exercise, can further exacerbate bone loss. Certain medical conditions, such as rheumatoid arthritis or hyperthyroidism, as well as medications like corticosteroids, can also increase your risk. Being aware of these factors allows you to make informed choices about your lifestyle and health.
Prevention and Management of Osteoporosis
| Metric | Description | Normal Range | Osteoporosis Threshold | Units |
|---|---|---|---|---|
| Bone Mineral Density (BMD) | Measurement of the amount of minerals (calcium) in a specific volume of bone | 1.0 or higher (T-score) | −2.5 or lower (T-score) | T-score (standard deviations) |
| Bone Mineral Content (BMC) | Total amount of mineral in bone | Varies by age and sex | Significantly reduced compared to age-matched controls | grams (g) |
| Trabecular Bone Score (TBS) | Assessment of bone microarchitecture quality | 1.350 or higher | Below 1.200 indicates degraded microarchitecture | Unitless |
| Serum Calcium | Calcium level in blood, important for bone health | 8.5 – 10.2 | May be normal or elevated in osteoporosis | mg/dL |
| Serum Vitamin D (25(OH)D) | Vitamin D level, essential for calcium absorption | 30 – 100 | Below 20 indicates deficiency | ng/mL |
| Fracture Risk Assessment Tool (FRAX) Score | 10-year probability of fracture | Varies by age, sex, and risk factors | Above 20% for major osteoporotic fracture considered high risk | Percentage (%) |
Preventing osteoporosis involves adopting a proactive approach to your bone health throughout your life. One of the most effective strategies is ensuring that you consume enough calcium and vitamin D daily. Foods rich in calcium include dairy products, leafy greens, and fortified foods, while vitamin D can be obtained through sunlight exposure and certain foods like fatty fish or fortified cereals.
If necessary, supplements can help you meet your nutritional needs. Incorporating regular physical activity into your routine is another vital aspect of prevention. Weight-bearing exercises such as walking, jogging, or resistance training stimulate bone formation and help maintain or even increase bone density.
Additionally, engaging in balance and flexibility exercises can reduce the risk of falls, which are a common cause of fractures in individuals with low bone density. By making these lifestyle changes early on, you can significantly reduce your risk of developing osteoporosis later in life.
Diagnosis and Testing for Osteoporosis

Diagnosing osteoporosis typically involves a combination of medical history assessment, physical examination, and diagnostic tests. One of the most common tests used to measure bone density is dual-energy X-ray absorptiometry (DEXA). This non-invasive test provides precise measurements of bone mineral density at key sites such as the hip and spine.
The results are then compared to standard values to determine whether you have normal bone density, low bone density (osteopenia), or osteoporosis. In addition to DEXA scans, your healthcare provider may consider other factors such as your age, sex, family history, and lifestyle when assessing your risk for osteoporosis. Blood tests may also be conducted to evaluate levels of calcium and vitamin D or to rule out other conditions that could affect bone health.
Early diagnosis is crucial for implementing effective management strategies and preventing further complications.
Treatment Options for Osteoporosis
If you are diagnosed with osteoporosis, several treatment options are available to help manage the condition and reduce the risk of fractures. Medications are often prescribed to help strengthen bones and slow down the rate of bone loss. Bisphosphonates are among the most commonly used medications; they work by inhibiting the cells that break down bone tissue, thereby increasing overall bone density.
In addition to medication, lifestyle modifications play a critical role in managing osteoporosis. Continuing with a balanced diet rich in calcium and vitamin D is essential for supporting bone health. Regular exercise should also be maintained or introduced if not already part of your routine; this includes both weight-bearing activities and exercises that improve balance and coordination.
Your healthcare provider may recommend working with a physical therapist to develop a safe exercise plan tailored to your needs.
Living with Osteoporosis: Tips for Daily Life
Living with osteoporosis requires adjustments to ensure safety and maintain quality of life. One of the most important aspects is fall prevention; since fractures are a significant concern for individuals with low bone density, taking steps to minimize fall risks is crucial. This may involve removing tripping hazards from your home, using non-slip mats, ensuring adequate lighting in all areas, and wearing supportive footwear.
Incorporating healthy habits into your daily routine can also make a significant difference in managing osteoporosis. Staying active through regular exercise not only helps maintain bone density but also boosts overall well-being. Additionally, staying connected with friends and family can provide emotional support and encouragement as you navigate living with this condition.
By prioritizing safety and adopting healthy habits, you can lead a fulfilling life while managing osteoporosis effectively.